Introduction
Understanding diabetic wound care is essential for maintaining foot and overall health as well.
In our comprehensive guide, learn essential tips and techniques to effectively manage and heal diabetic wounds, either employing a diabetic wound gel, creams, ointments, or other resources to ensure optimal health and well-being.
Empower yourself with the knowledge to prioritize diabetic wound care confidently and prevent complications.
Causes for Diabetic Wounds
Generally speaking, wounds and ulcers onset because of diverse factors:
- Diminished foot sensation: Diabetes-induced neuropathy reduces foot sensitivity, delaying injury detection
- Poor blood circulation: Diabetes damages blood vessels, slowing wound healing
- Foot abnormalities: Structural changes increase pressure points, leading to ulcerations
- Irritation from friction or pressure: Ill-fitting footwear or clothing can cause skin breakdown, fostering ulcers
- Prolonged diabetes duration: Longer diabetes duration heightens neuropathy and vascular complications, increasing the risk for ulcers
- Neuropathy: Since nerve damage impairs pain perception in the feet and other limbs, wounds often develop painlessly, making detection challenging without a sound professional assessment
- Vascular issues: These exacerbate foot ulcers and bodily wounds, hindering healing and elevating infection risks
- Elevated blood glucose levels: They compromise the body’s infection-fighting capabilities and slow down wound-healing processes
Symptoms
Due to diminished pain sensation in individuals with wounds, pain isn’t frequently experienced, making detection harder.
Initial signs often include drainage on clothing such as socks, accompanied by redness and swelling near the ulceration site. In advanced stages, odor may become noticeable as well.
Whenever you notice any of these signs, it is imperative to seek professional assistance.
Treatment
The primary objective in treating wounds and ulcers is prompt healing. This minimizes infection risks. Some key components of diabetic foot ulcer management include the following:
- Infection prevention
- Off-loading pressure from the affected area, especially on foot undersides
- Removing dead tissue
- Employing special footwear, braces, castings, or mobility aids to reduce pressure and facilitate recovery
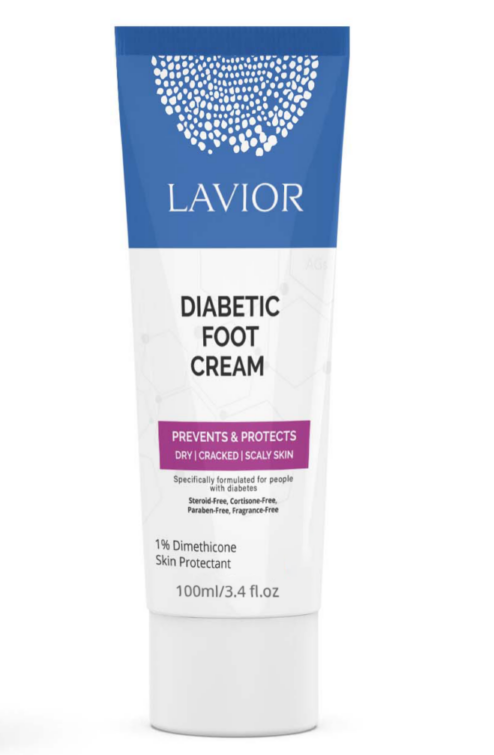
- Applying appropriate medication or dressings. Lavior products are quintessential for this matter
- Managing overall health conditions like blood glucose levels
Not all ulcers are infected, but if diagnosed as such, a treatment regimen involving antibiotics, wound care, and even possible hospitalization is necessary. Preventing infection involves maintaining tight control over blood glucose levels, keeping the ulcer clean and bandaged, daily wound cleansing, and avoiding barefoot walking altogether.
If the exposed area is not a foot, it is usually easier to deal with, as the foot usually has many pressure points that hinder healing processes.
In general, avoiding practices like the use of full-strength betadine, hydrogen peroxide, whirlpools, or soaking is crucial to prevent problems. Adequate circulation to the ulcerated area is vital for healing, assessable through non-invasive podiatrist tests. Try our specialized Diabetic Foot Cream for regular care.
Take Care of Your Wounds Adequately and Promptly
Lack of adequate wound treatment can lead to further problems, such as wound infection or other health-derived issues that can easily be tackled with our dedicated line of gels and ointments.
Lavior is a company that creates top-notch, ADA-approved ointments for wound care and foot and leg ulcerations.