Diabetes is a chronic condition characterized by high blood sugar levels, and affects millions worldwide. Although the effects of diabetes on organs such as the eyes and kidneys are well-known, there is a less recognized but potentially severe consequence called diabetic wounds.
A Prevalence We Can’t Ignore:
According to the International Diabetes Federation’s figures, foot ulcers affect an estimated 9.1 million to 26.1 million diabetics globally each year. Studies suggest that roughly 15% to 25% of individuals with diabetes will develop a foot ulcer at some point in their lives. This risk increases with the duration and severity of the disease. Recent findings indicate a significant rise in the number of amputations in certain areas. This increase is particularly notable among young individuals and racial and ethnic minority groups.
The Harsh Effects Take Many Forms:
An article published in the New England Journal of Medicine reported that Patients with diabetic foot ulcers have a 2.5 times higher risk of death at five years compared to those without the ulcer. Furthermore, more than 50% of diabetic ulcers become infected, and 20% of mild or severe diabetic foot infections require amputation. Similarly, the quality of life with diabetes foot ulcers is jeopardized. Not only the patients but caregivers also suffer from psychological, emotional and financial traumas.
It is also estimated the average annual cost of diabetic foot care is $8659 per patient. The entire medical cost of treating diabetic foot illnesses in America is from $9 to $13 billion, which is an additional cost linked with diabetes.
Unmasking the Risk Factors:
Several factors contribute to the development of diabetic wounds including
- Poor blood sugar control:Chronically high blood sugar levels impair healing and weaken the immune system, making infections more likely.
- Nerve damage (neuropathy):This can lead to a loss of sensation, making it difficult to notice injuries like cuts or blisters, allowing them to worsen unnoticed.
- Poor circulation:Diabetes can narrow blood vessels, restricting blood flow, which slows healing and hinders oxygen and nutrient delivery to the wound site.
- Smoking:Further compromises circulation and impairs wound healing.
Managing the Threat
Foot ulcers can often be healed with adequate therapy, including surgical debridement, pressure off-loading, infection control, and vascular reconstruction, preventing the need for amputation. Medical research shows that 77% of diabetic foot ulcers heal within a year. However, for this means taking extra care that include
- Meticulous blood sugar control:Maintaining optimal blood sugar levels is crucial for preventing complications.
- Regular checkups:Early detection and treatment of foot problems by a healthcare professional are vital.
- Healthy lifestyle:Quitting smoking, maintaining a healthy weight, and engaging in regular physical activity can improve circulation and overall health.
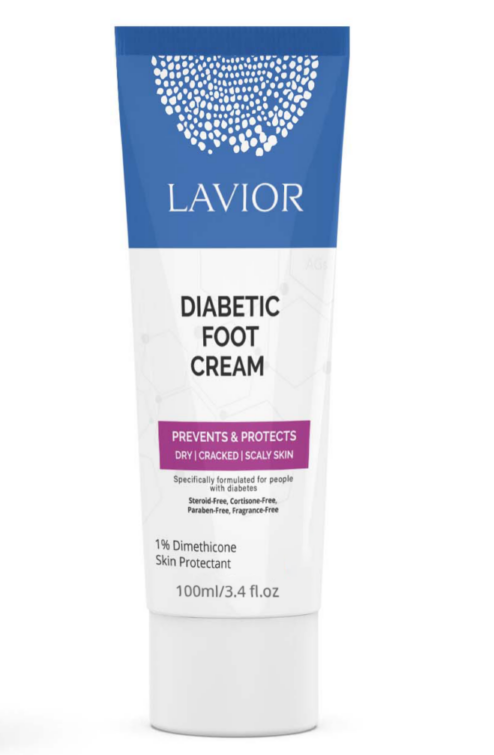
- Foot care:Daily inspections for injuries, proper moisturizing, and comfortable footwear are essential. Even minor cuts or scrapes can turn into serious problems if not managed properly. That’s where Lavior Diabetic Wound Gel comes in.
More than just a gel; it’s a shield and a healer. Formulated specifically for diabetic individuals for proper foot care
Lavior goes beyond the basics. Its active ingredient is Allantoin 0.5%. It does not just treat the wound, and it creates the optimal environment for your skin to regenerate. Allantoin is known for its moisturizing and keratolytic effects, which help to increase the water content of the extracellular matrix and enhance cell proliferation. With a unique blend of natural ingredients works in harmony to promote healthy blood flow, fight infection and, reduce inflammation and prevent harsh consequences.
Taking care of your diabetic wounds doesn’t have to be complicated. Lavior makes it easy.
Don’t wait; reclaim your well-being today with Lavior Diabetic Wound Gel. Click here and take charge of your foot health today.
Sources:
Atlas, D. (2015). International diabetes federation. IDF Diabetes Atlas, 7th edn. Brussels, Belgium: International Diabetes Federation, 33(2).
Armstrong, D. G., Boulton, A. J., & Bus, S. A. (2017). Diabetic foot ulcers and their recurrence. New England Journal of Medicine, 376(24), 2367-2375.
Zhang, P., Lu, J., Jing, Y., Tang, S., Zhu, D., & Bi, Y. (2017). Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis. Annals of medicine, 49(2), 106-116.
Mutluoglu, M., Uzun, G., Turhan, V., Gorenek, L., Ay, H., & Lipsky, B. A. (2012). How reliable are cultures of specimens from superficial swabs compared with those of deep tissue in patients with diabetic foot ulcers?. Journal of diabetes and its complications, 26(3), 225-229.
Prompers, L., Schaper, N., Apelqvist, J., Edmonds, M., Jude, E., Mauricio, D., … & Huijberts, M. (2008). Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. The EURODIALE Study. Diabetologia, 51, 747-755.