Untreated itchy skin, also known as puritus, can have serious consequences in persons with diabetes. Chronic scratching can cause skin thickening, or scarring. Additionally, constant scratching can lead to breaks in the skin allowing bacteria to enter into the deeper tissues and cause infection. On occasion these infections can become severe, requiring antibiotics or long-term therapy. Moreover, this constant skin irritation may take an emotional toll on the patient contributing to higher stress levels and worsened diabetes control, creating a vicious cycle.
Puritus is an uncommon symptom of diabetes, a complicated disorder wherein your blood sugar is just too excessive. Diabetic itching can be a result of dry skin, improper blood circulation, or specific infections. It might additionally disturb and interfere with patient daily activites.
Itching Effecting Millions Of Individuals With Diabetes
Approximately 79% of individuals who experience diabetes mellitus, face skin issues including dryness, infections, and itching. Those can arise at any point throughout the disease. In a few cases, skin issues can also be the primary sign that someone has diabetes (1). A published study in the medical journal Advances in Dermatology and Allergology reported that itching is prevalent in up to 27.5% of diabetic individuals (2). According to the International Diabetes Federation (IDF), the prevalence of diabetes is around 500 million worldwide.With more that 100 million individuals diagnosed with this disease (3).
Itchy Skin and Mental Health in Diabetes
Many of us know the frustration of an itchy rash, but for people with diabetes, this itch can be more than just annoying – it can be linked to anxiety and depression. A recent study published in a renowned medical journal Biology found that diabetic individuals patients experiencing itchiness were 6 times more likely to have anxiety compared to those without it. And while depression wasn’t quite as prevalent, it still affected 7.6% of itchy patients compared to only 1.4% in the non-itchy group (4).These findings highlight a concerning connection between skin issues and mental well-being in patients with Non-Insulin Dependant Diabetes.
Economic Impact of Chronic Itch Are In Billions of USD $
While the social ramifications of chronic itch are often experienced in isolation and shame, the true impact goes much deeper. Studies reveal a significant decrease in quality of life (QoL) for individuals struggling with this persistent condition. Even conservative estimates, based on willingness-to-pay models, show a substantial economic burden of $274,921 per individual over their lifetime (5). Another medical publication noted that patients suffering from chronic skin itch pay an average of $1,067 in direct and indirect healthcare costs each year including spending on things such as medical visits, including tests, procedures, medications, and transportation costs (6).
What Causes Itching In Diabetic Patients
There are numerous causes of of skin itch in individuals with diabetes and some people may observe more severe symptoms than others. The following are the some common reasons for skin itching in persons with diabetes.
Neuropathy
Diabetic neuropathy, or nerve damage, can cause chronic itch and neuropathic discomfort. Diabetic neuropathy is the most prevalent systemic complication of diabetes. A growing body of evidence indicates nerve inflammation is a pivotal factor in the pathophysiology of chronic skin itch and neuropathic pain. Eventually, individuals may observe other abnormal sensations, including burning, and tingling, numbness or cold sensations as a result of nerve damage. Individuals who are affected by diabetic neuropathy and lack feeling in there feet and hands may develop blisters from repetitive rubbing or pressures on the skin. Diabetic blisters can occur on any skin surface but are most common on the bottoms of the feet, toes, fingers or legs.
Poor Circulation
Diabetes can also affect circulation by reducing blood supply to various body components, including the skin. This reduced blood supply can lead to skin changes such as dryness, fissures, and rashes. Decreased circulation may also disturb the body’s potential to heal, increasing the threat of infections.
Skin Dryness
Skin dryness is a common issue with diabetic skin. If blood sugar is not adequately managed, it could result in dehydration, affecting your skin’s moisture barrier. Dry skin is generally more susceptible to itching because it lacks the natural defensive barrier that healthy skin provides.
Knowing these underlying causes of diabetic itching is vital for finding ways to relieve it. Not only can the mentioned factors trigger itching, but they can also worsen the condition if left untreated. By addressing these root causes, you can take significant steps toward identifying appropriate remedies.
Associated Diabetic Skin Conditions
In some cases, an underlying skin disorder can lead to itching. People with diabetes are more likely to experience skin problems and infections than those without diabetes.
Examples of such conditions include:
- Fungal infections
- Eruptive xanthomatosis
- Necrobiosis lipoidica diabeticorum (NLD)
What to DO !
Let’s have a look at various steps to relieve diabetic itching.
- Maintain Blood Sugar balance
- Attend routine check-ups by health practitioner
- Preserve skin Moisture
- Use Diabetic Itch Relief Cream
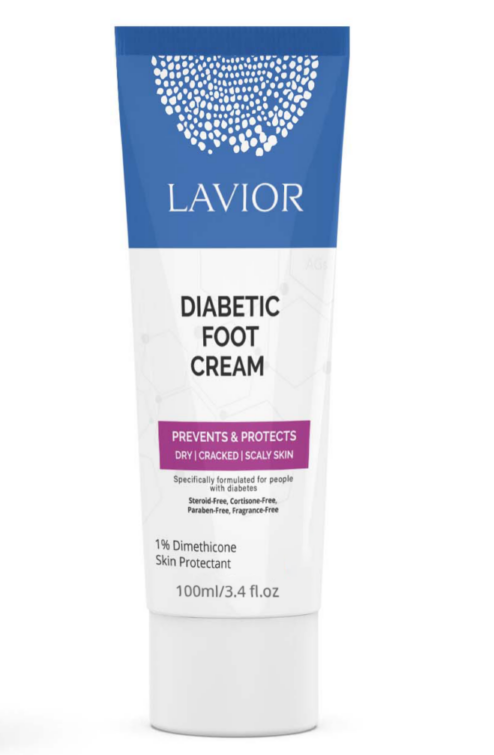
If you’re tired of dealing with the discomfort and irritation that comes with dry, itchy skin, try Lavior’s Diabetic Itch Relief Cream. It contains a unique blend of moisturising nutrients like as shea butter and aloe vera, absorbs rapidly and provides long-lasting relief without leaving any residue. The best thing is that Lavior’s Diabetic Itch Relief Cream is formulated with diabetic skin in mind, and is dermatologist-tested and recommended.
If your itching persists or becomes severe even after following those remedies and training in proper diabetes management, seek advice from your healthcare expert.
References:
- Fang, X. X., Wang, H., Song, H. L., Wang, J., & Zhang, Z. J. (2022). Neuroinflammation involved in diabetes-related pain and itch. Frontiers in Pharmacology, 13, 921612.
- Stefaniak, A., Chlebicka, I., & Szepietowski, J. (2019). Itch in diabetes: a common underestimated problem. Advances in Dermatology and Allergology/Postępy Dermatologii i Alergologii, 38(2), 177-183.
- International Diabetes Federation: https://idf.org/about-diabetes/diabetes-facts-figures/
- Stefaniak, A. A., Krajewski, P. K., Bednarska-Chabowska, D., Bolanowski, M., Mazur, G., & Szepietowski, J. C. (2021). Itch in adult population with type 2 diabetes mellitus: clinical profile, pathogenesis and disease-related burden in a cross-sectional study. Biology, 10(12), 1332.
- Whang, K. A., Khanna, R., Williams, K. A., Mahadevan, V., Semenov, Y., & Kwatra, S. G. (2021). Health-related QOL and economic burden of chronic pruritus. Journal of Investigative Dermatology, 141(4), 754-760.
- Luk, K. M., Shaw, F. M., Zhang, C., Culler, S. D., & Chen, S. C. (2019). The Annual Direct and Indirect Health Care Costs for Patients with Chronic Pruritus and their Determining Factors. The Journal of Investigative Dermatology, 140(3), 699-701.